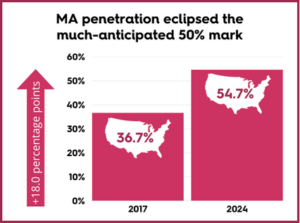
 As Medicare Advantage (MA) continues its rapid expansion—now covering nearly 55% of all Medicare-eligible beneficiaries as of early 2024—healthcare providers must refine their strategies to remain competitive. With the shift away from traditional fee-for-service models, the ability to negotiate, manage, and optimize MA contracts is becoming a vital differentiator for success.
As Medicare Advantage (MA) continues its rapid expansion—now covering nearly 55% of all Medicare-eligible beneficiaries as of early 2024—healthcare providers must refine their strategies to remain competitive. With the shift away from traditional fee-for-service models, the ability to negotiate, manage, and optimize MA contracts is becoming a vital differentiator for success.
In a recent webinar, Navigating Medicare Advantage Contracts: Leveraging Data for Smarter Contracting Decisions, industry experts explored the challenges and opportunities of the MA landscape and how providers can use data to secure more favorable contract terms, improve care coordination, and drive sustainable growth.
The Growing Importance and Complexity of MA Contracts
While MA plans offer new pathways for patient engagement and care delivery, they come with unique challenges. These include:
- Unpredictable patient volumes
- Variable reimbursement rates
- Stringent utilization management practices
- Frequent policy changes
To navigate this complexity, providers must embrace data-driven decision-making at every stage of the contracting process—from identifying the right plans to forming physician relationships and tracking performance metrics.
Best Practices for Optimizing Medicare Advantage Contracts
Identify High-Value MA Plans in Your Market
Not all MA plans are created equal. Some may offer wide patient coverage but low utilization for home health or Skilled Nursing Facilities (SNF) services. Others may come with burdensome administrative requirements or declining enrollment. Providers should:
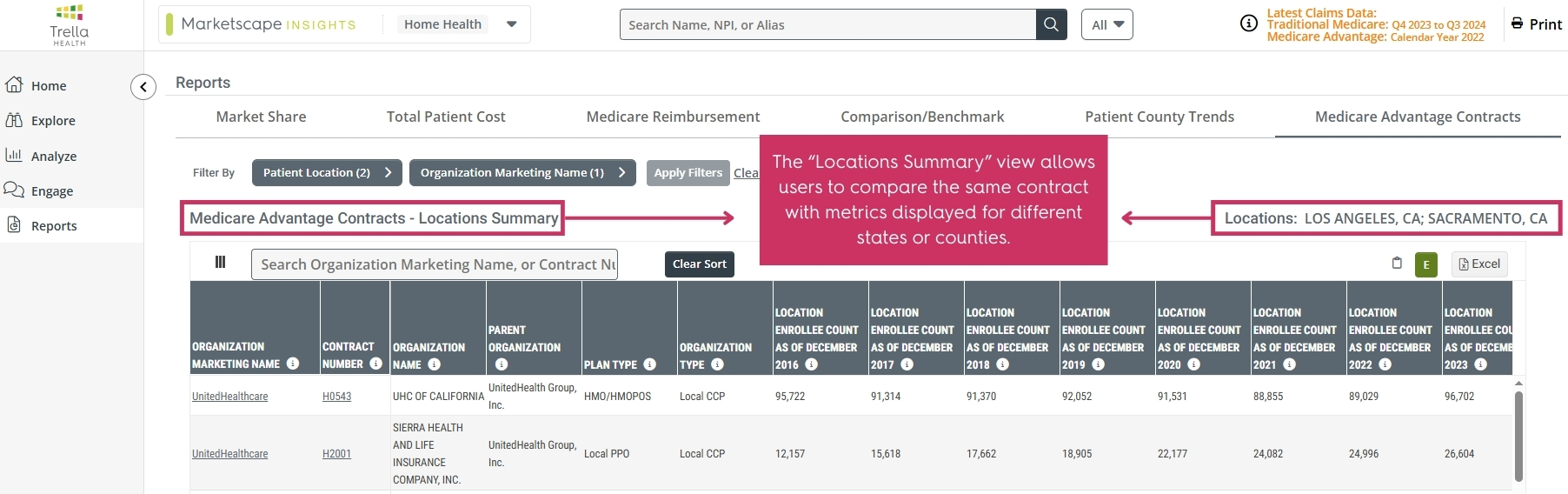
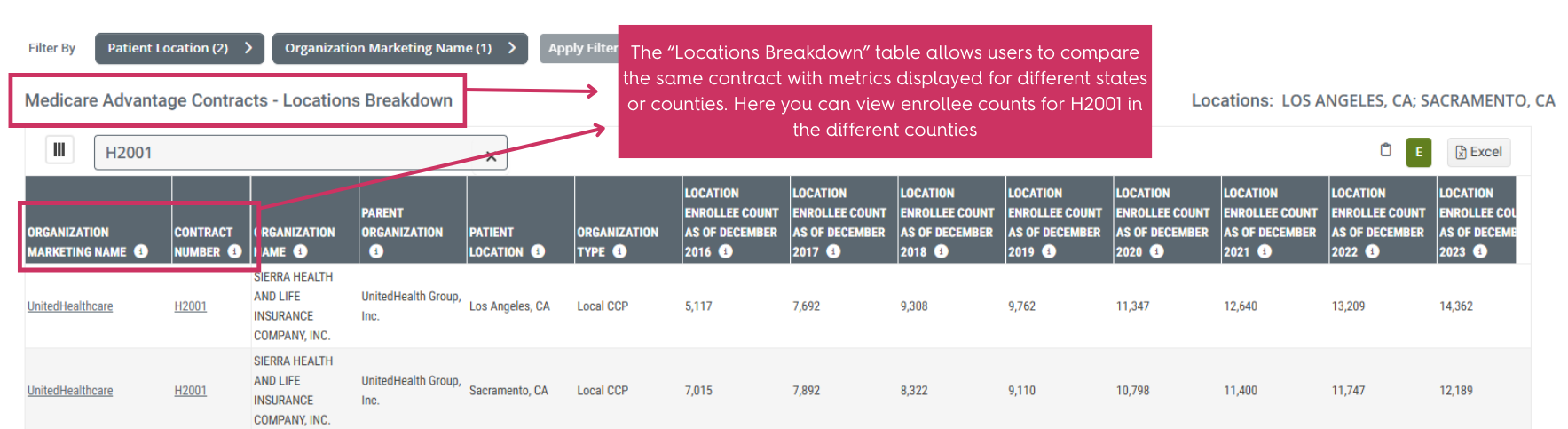
- Use tools like Trella Health’s Marketscape Insights to access timely enrollment and utilization trends.
- Track plan performance by county to target those with higher post-acute service utilization.
- Prioritize plans aligned with value-based care and long-term sustainability.
Negotiate Smarter, Data-Backed Contracts
Many MA plans offer lower reimbursement rates than traditional Medicare, with no standardized pricing. To strengthen negotiating power, providers should:
- Present data demonstrating cost savings through reduced hospital readmissions and efficient care transitions.
- Compare performance benchmarks against peers to showcase their unique value.
- Align contracts with financial goals and care priorities while pushing for transparent terms and minimal administrative burden.
Prove Value with Measurable Outcomes
MA plans focus heavily on reducing costs and improving outcomes. Providers who can demonstrate their positive impact on both fronts have a stronger case for better contracts.
For example:
- Home health agencies that reduce readmissions can argue for higher reimbursement rates.
- SNFs with strong rehabilitation outcomes can position themselves as preferred partners.
- Using data to quantify outcomes—like patient satisfaction, recovery times, or avoided hospitalizations—can significantly boost credibility during negotiations.
Strengthen Physician and Referral Networks
Referrals are critical in the MA environment due to narrower provider networks. To grow within MA plans:
- Identify physicians with high MA patient volumes.
- Assess referral patterns using analytics to enhance engagement with top-performing providers.
- Share performance data and success stories to build trust with referring physicians.
Avoid Low-Value or Underperforming Contracts
Not every MA contract is worth pursuing. Low-value contracts can drain resources and reduce profitability. Providers should:
- Evaluate enrollment and utilization trends to determine viability.
- Flag contracts with heavy documentation burdens or declining member numbers.
- Focus efforts on plans that deliver both financial return and patient care alignment.
Adapt to a Changing MA Landscape
MA policies and reimbursement models are constantly evolving, making long-term planning a challenge. To stay proactive:
- Monitor CMS announcements and policy updates.
- Be prepared to renegotiate contracts when policies shift.
- Use predictive data to anticipate utilization or reimbursement changes before they impact your bottom line.
Using Data to Drive Strategic Growth
Data is the key to unlocking smarter Medicare Advantage contracting. Trella Health’s Medicare Advantage Contracts feature provides organizations with a clear, consolidated view of:
- MA plan enrollment trends
- Post-acute utilization patterns
- Physician referral networks
With these insights, providers can:
- Identify growth opportunities
- Optimize contract negotiations
- Build targeted partnerships
- Enhance their market position
Turning Insight into Action
Medicare Advantage presents both a challenge and a significant opportunity. Providers who invest in the right data tools and strategic relationships will be better positioned to succeed in this growing market. Whether you’re renegotiating a contract, seeking new partnerships, or evaluating your current MA plan performance, a data-driven approach is no longer optional—it’s essential.
Ready to grow smarter with your Medicare Advantage strategy?
Explore how Trella Health can help you make more informed decisions. Request a demo today.